Testosterone. The very word carries an aura of power, energy, and vitality—sometimes even a hint of danger. It’s the hormone that fuels competition, muscles, and motivation. But beyond the myths and macho marketing, testosterone is a biological cornerstone of male physiology and mental health. Understanding what it truly does, how it fluctuates, and why modern men are facing declining levels is not just an academic exercise—it’s a survival guide for modern masculinity.
Let’s break it down scientifically, without forgetting that biology can also be fascinating (and occasionally funny).
Definition
Testosterone is a steroid hormone primarily produced in the Leydig cells of the testes in men, and in smaller quantities by the ovaries in women and the adrenal cortex of both sexes. Chemically, it belongs to the class of androgens—hormones that stimulate the development of male characteristics. Its molecular formula, C₁₉H₂₈O₂, may not look like much, but this small molecule orchestrates a symphony of physiological effects.
It’s responsible for the development of male reproductive tissues, such as the testes and prostate, as well as secondary sexual characteristics like increased muscle mass, bone density, and the growth of body hair. But testosterone also has profound effects on the brain—it influences mood, motivation, risk-taking, and even the perception of dominance.
Interestingly, women also produce testosterone—about one-tenth to one-twentieth of male levels—and it plays a critical role in libido, energy, and muscle tone. So no, testosterone isn’t just for the guys; it’s just more abundant in them.
How Much Testosterone Should We Have (by Age/Sex)
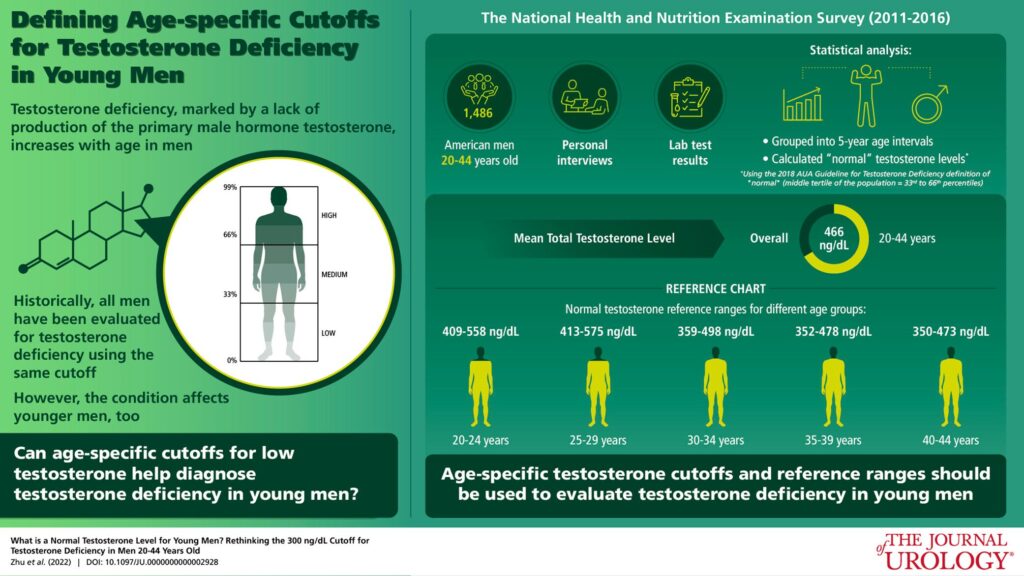
Normal testosterone levels vary widely, but generally, adult males range between 300 to 1,000 nanograms per deciliter (ng/dL), while adult females range between 15 to 70 ng/dL. However, numbers are only half the story. A man with 400 ng/dL might feel amazing, while another with 600 might feel chronically tired—it’s about how your body uses that testosterone.
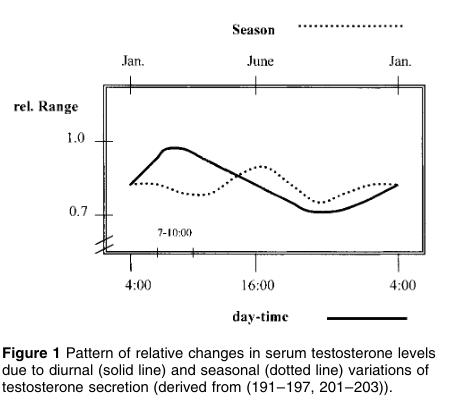
Levels naturally peak in early adulthood (around age 20) and start to decline gradually—by about 1% per year after age 30 (Harman et al., 2001, Journal of Clinical Endocrinology & Metabolism). By the time a man reaches his 50s or 60s, it’s perfectly normal for his testosterone to be significantly lower than in his twenties.
However, “normal” does not necessarily mean “optimal.” Population averages are skewed by unhealthy lifestyles, poor diets, and sedentary habits—factors that suppress hormone production. Therefore, the range of “healthy” testosterone in today’s average male might reflect a generation that sleeps poorly, eats junk, and moves little.
Optimal Testosterone Levels by Age and Sex
Below is a reference table showing average and optimal total testosterone levels (ng/dL) by sex and age group, based on population data and clinical research (Harman et al., 2001; Bhasin et al., 2018, Endocrine Society Guidelines).
Men
| Age Range | Optimal Total Testosterone (ng/dL) | Clinical Notes |
|---|---|---|
| 18–25 years | 600 – 1,000 | Peak natural production; levels above 800 linked to optimal muscle mass and libido. |
| 26–35 years | 550 – 950 | Slight decline begins; lifestyle strongly influences hormone balance. |
| 36–45 years | 500 – 900 | About 1% annual decrease; maintenance depends on sleep and strength training. |
| 46–55 years | 400 – 850 | Noticeable decline; levels below 400 often associated with clinical symptoms. |
| 56–65 years | 350 – 800 | Natural aging effect; TRT may be considered when symptomatic. |
| 66–75 years | 300 – 750 | Still healthy if symptoms are absent; below 300 usually signals hypogonadism. |
| 76+ years | 250 – 700 | Strongly dependent on overall health, medications, and metabolic stability. |
Women
| Age Range | Optimal Total Testosterone (ng/dL) | Clinical Notes |
|---|---|---|
| 18–25 years | 30 – 70 | Peak reproductive phase; highest natural levels of life. |
| 26–35 years | 25 – 65 | Stable phase; oral contraceptives may reduce levels. |
| 36–45 years | 20 – 60 | Gradual decline before menopause. |
| 46–55 years | 15 – 50 | Perimenopause drop; low libido and fatigue common. |
| 56+ years | 10 – 40 | Postmenopausal range; values under 15 suggest androgen deficiency. |
Additional Notes
- Free Testosterone: represents 1–3% of total testosterone and is the biologically active fraction.
Men: 5 – 20 ng/dL
Women: 0.3 – 1.9 ng/dL - SHBG (Sex Hormone-Binding Globulin): High SHBG reduces free testosterone availability.
- Reference ranges vary between labs (±20%). Always interpret results in combination with clinical symptoms.
Sources: Harman et al., 2001; Bhasin et al., 2018; Travison et al., 2007; Endocrine Society Clinical Practice Guidelines.
Is Testosterone Declining Nowadays?
Short answer: yes. Longer answer: alarmingly yes.
Several large-scale studies, including the Massachusetts Male Aging Study (Travison et al., 2007, Journal of Clinical Endocrinology & Metabolism), have shown a steady decline in average testosterone levels among men over the past few decades—even after adjusting for age. In other words, a 40-year-old man today has significantly less testosterone than a 40-year-old man in the 1980s.
Researchers suspect multiple culprits: increased obesity, poor diet, chronic stress, sleep deprivation, environmental toxins, and endocrine-disrupting chemicals found in plastics and personal-care products. Yes, your shampoo might be lowering your testosterone.
Sedentary lifestyles also play a role. Humans were designed to hunt, fight, build, and move. Instead, most men today spend ten hours sitting in front of screens, consuming processed food, and scrolling through digital dopamine hits. That combination is, quite literally, the opposite of what the male endocrine system evolved for.
How Lifestyle Can Impact Testosterone Levels
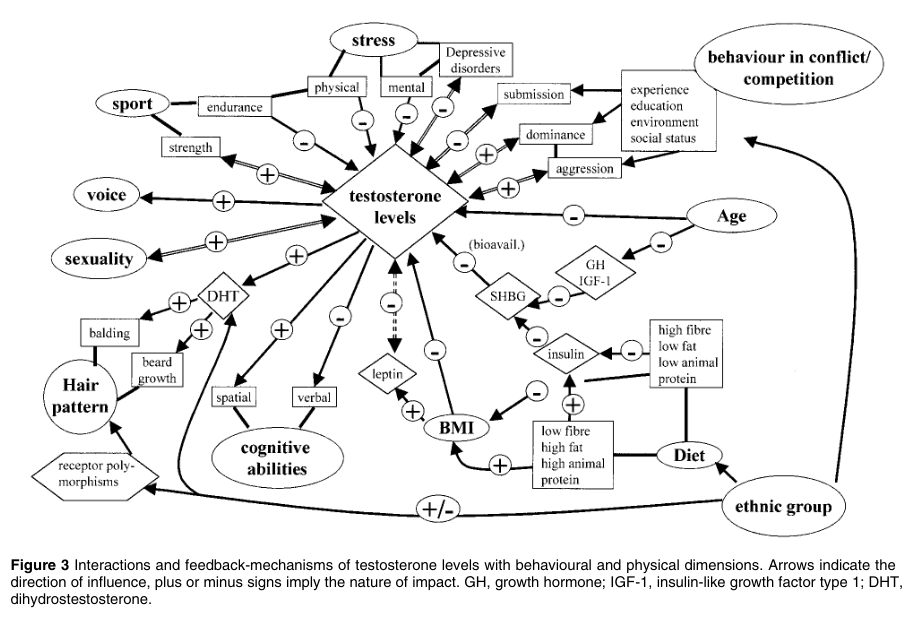
Testosterone production is deeply connected to lifestyle. Sleep, nutrition, exercise, and even psychological stress all influence the hypothalamic-pituitary-gonadal (HPG) axis—the control system that regulates testosterone.
Sleep deprivation is one of the most potent natural testosterone killers. In a landmark study by Leproult and Van Cauter (2011, JAMA), young men who slept only five hours per night for one week showed a 10–15% drop in testosterone. Imagine losing a decade of hormonal vitality just because you binge-watched another season of your favorite series.
Diet is another major factor. Testosterone synthesis depends on adequate levels of zinc, magnesium, vitamin D, and cholesterol. Yes—cholesterol. That’s because all steroid hormones, including testosterone, are derived from it. This is why ultra-low-fat diets can lead to low testosterone.
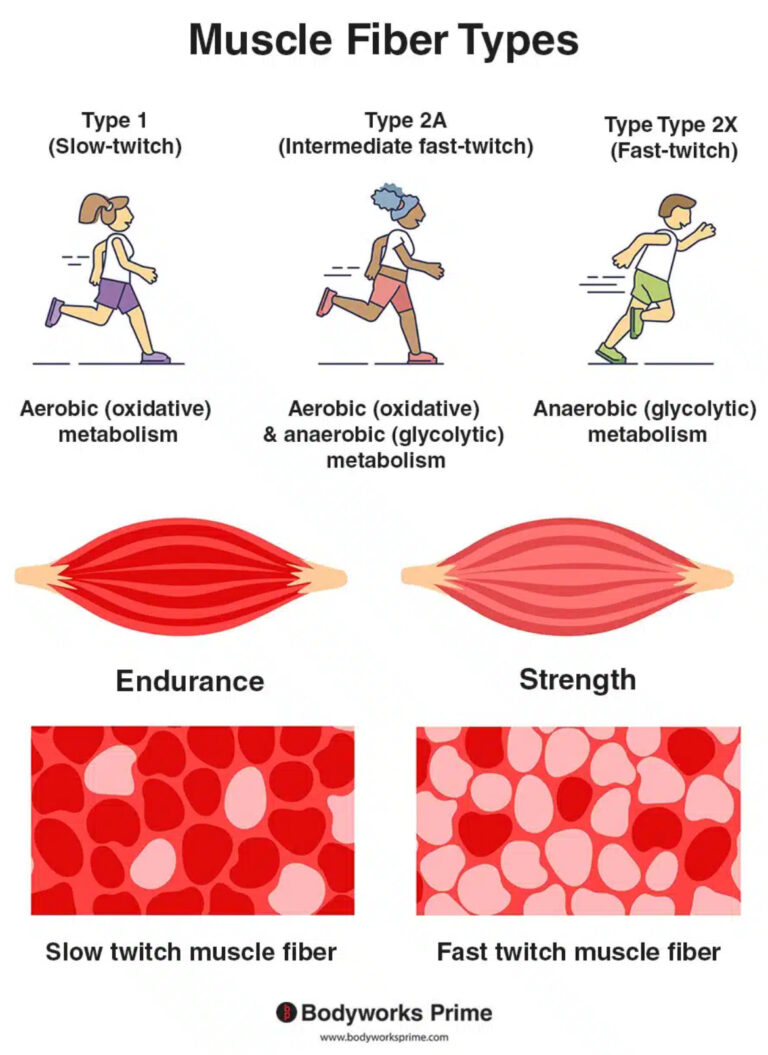
Resistance training—especially compound lifts like squats and deadlifts—has been shown to increase testosterone temporarily. On the other hand, chronic endurance training, such as long-distance running, can suppress testosterone if recovery is insufficient.
Chronic stress releases cortisol, which directly inhibits testosterone production. It’s almost as if your body says, “You seem to be running from lions—this is no time for reproduction.” Unfortunately, today’s “lions” are emails, deadlines, and bills.
Why Athletes Take Testosterone and Other Hormones to Improve Performance
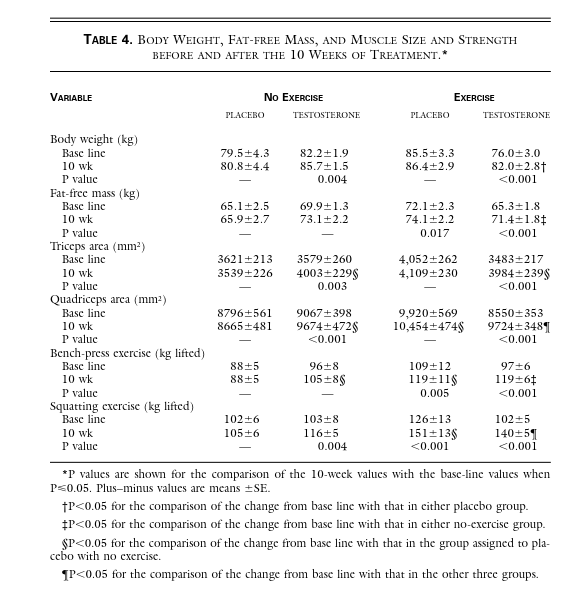
Let’s not be naïve—testosterone is powerful. Athletes use it because it works. Exogenous testosterone (administered from outside the body) can increase muscle mass, reduce body fat, and accelerate recovery dramatically.
Testosterone enhances protein synthesis, which means your muscles repair and grow faster after training. It also increases red blood cell production, improving oxygen delivery to muscles—translating into better endurance and less fatigue.
That’s why testosterone and its derivatives have been the cornerstone of performance-enhancing drug (PED) use in sports since the 1950s. The Soviet Union, East Germany, and later professional bodybuilders and athletes across disciplines all recognized its power.
Of course, these effects come at a price. Excessive doses can cause infertility, cardiovascular issues, mood swings, and irreversible endocrine damage. So while testosterone might make you stronger, abusing it can make you medically miserable.
Still, the underlying truth remains: testosterone is performance-enhancing because it enhances the very machinery of human vigor.
What Is TRT?
Testosterone Replacement Therapy (TRT) is the medical administration of testosterone to restore physiological levels in men who are clinically deficient. It’s not the same as steroid abuse—TRT aims to bring you back to normal, not transform you into a comic book character.
TRT can be delivered via injections, gels, patches, or pellets implanted under the skin. The goal is to maintain steady testosterone levels and alleviate symptoms of low testosterone—such as fatigue, depression, loss of libido, poor concentration, and reduced muscle mass.
Several studies support the benefits of TRT. Men receiving treatment often report improved mood, energy, sexual function, and even cognitive performance (Saad et al., 2017, Aging Male). Additionally, TRT can increase bone density and muscle mass while reducing fat accumulation.
However, it’s not a free pass to eternal youth. Improper management of TRT can lead to issues like erythrocytosis (too many red blood cells), suppression of natural testosterone production, or imbalance in estrogen levels. That’s why medical supervision is crucial—ideally with professionals who understand both the science and the art of hormonal optimization.
A Brief Word on Fear and Stigma
Despite growing awareness, TRT and testosterone optimization still face cultural stigma. Many men are reluctant to seek treatment because they fear being labeled as “cheaters” or “vain.” Yet, no one hesitates to take thyroid medication when their T4 is low. Why should testosterone be any different?
This double standard keeps countless men suffering from fatigue, anxiety, and loss of vitality—all because of a societal myth that “real men” should tough it out. In truth, real men take responsibility for their health, whether that means fixing their diet, sleeping more, or restoring their hormones to optimal levels.
The Psychology of Testosterone
Beyond its physical effects, testosterone profoundly influences confidence, motivation, and resilience. Men with higher testosterone tend to take more initiative, pursue challenges, and show greater persistence in competitive environments (Archer, 2006, Neuroscience & Biobehavioral Reviews).
This doesn’t mean testosterone makes you aggressive—it makes you driven. The stereotype of the “roid-raging” bodybuilder is exaggerated. What testosterone really does is increase the desire to achieve status and competence. In other words, it doesn’t make you violent—it makes you ambitious.
Low testosterone, on the other hand, is often associated with apathy, low self-esteem, and even depressive symptoms. It’s not just about muscles—it’s about mental sharpness and emotional balance.
A Modern Epidemic
If you feel constantly tired, unmotivated, and unfocused, don’t rush to blame your job or your smartphone addiction (although both could be suspects). Low testosterone has become a modern epidemic. The average man today is weaker, fatter, and less energetic than his grandfather—and not because of genetics, but lifestyle.
Low T is a signal from your body that something is fundamentally off—poor sleep, nutritional deficiencies, lack of physical challenge, or chronic stress. You can’t fake biology; your hormones reflect your habits.
How to Fix It (Naturally, If Possible)
Start with the basics:
- Sleep at least 7–8 hours per night.
- Lift weights regularly, focusing on large muscle groups.
- Eat whole foods rich in healthy fats and micronutrients.
- Avoid chronic calorie restriction and extreme endurance exercise.
- Reduce stress and exposure to endocrine disruptors.
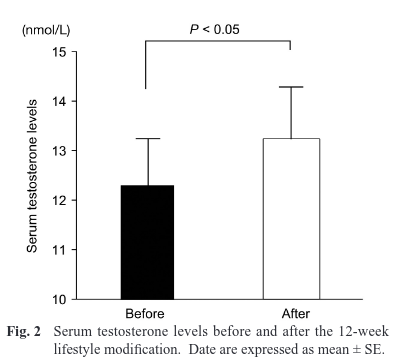
These steps alone can significantly improve testosterone levels. In fact, studies show that obese men who lose weight through diet and exercise can increase their testosterone by up to 30% (Khoo et al., 2013, Clinical Endocrinology).
If, after all that, your levels are still low, then TRT under professional supervision may be the right path.
Conclusion: Testosterone Is Not Just a Hormone—it’s the Spark of Manhood
Testosterone fuels more than muscles; it fuels meaning. It gives men the biological foundation for drive, protection, creation, and passion. Without it, both the body and the spirit fade into lethargy.
The modern world is not designed for high testosterone—it rewards convenience, comfort, and compliance. But biology doesn’t care about social trends. Your body still expects you to fight, lift, lead, and protect.
Understanding testosterone—and managing it wisely—is not vanity. It’s self-respect.
Need Guidance? Let’s Talk Science, Not Myths.
If you suspect your hormones are out of balance, don’t play doctor with internet advice. Our team at Forge Biology offers personalized consultancy based on medical evaluation, lab interpretation, and evidence-based lifestyle optimization.
Whether you’re struggling with fatigue, performance plateaus, or just want to feel like yourself again—we can help you forge your biology back into balance.
Book your consultation today and start reclaiming your strength, focus, and vitality—scientifically.
References
Archer, J. (2006). Testosterone and human aggression: An evaluation of the challenge hypothesis. Neuroscience & Biobehavioral Reviews, 30(3), 319–345.
Bhasin, S., Storer, T. W., Berman, N., Callegari, C., Clevenger, B., Phillips, J., … & Casaburi, R. (1996). The effects of supraphysiologic doses of testosterone on muscle size and strength in normal men. New England Journal of Medicine, 335(1), 1-7.
Harman, S. M., Metter, E. J., Tobin, J. D., Pearson, J., & Blackman, M. R. (2001). Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Journal of Clinical Endocrinology & Metabolism, 86(2), 724–731.
Khoo, J., et al. (2013). Comparing effects of low- and high-carbohydrate diets on testosterone levels and metabolic outcomes in obese men. Clinical Endocrinology, 78(3), 432–439.
Kumagai, H., Zempo-Miyaki, A., Yoshikawa, T., Tsujimoto, T., Tanaka, K., & Maeda, S. (2015). Lifestyle modification increases serum testosterone level and decrease central blood pressure in overweight and obese men. Endocrine journal, 62(5), 423-430.
Leproult, R., & Van Cauter, E. (2011). Effect of 1 week of sleep restriction on testosterone levels in young healthy men. JAMA, 305(21), 2173–2174.
Saad, F., Aversa, A., Isidori, A. M., & Gooren, L. J. (2017). Testosterone as potential effective therapy in treatment of obesity in men with testosterone deficiency: A review. Aging Male, 20(1), 1–11.
Travison, T. G., Araujo, A. B., O’Donnell, A. B., Kupelian, V., & McKinlay, J. B. (2007). Decline in serum testosterone levels among American men. Journal of Clinical Endocrinology & Metabolism, 92(1), 196–202.
M Zitzmann, E Nieschlag, Testosterone levels in healthy men and the relation to behavioural and physical characteristics: facts and constructs, European Journal of Endocrinology, Volume 144, Issue 3, Mar 2001, Pages 183–197, https://doi.org/10.1530/eje.0.1440183
Forge Your Mind. Build Your Biology.
Join the Forge Biology newsletter — where science meets strength.
Every week, you’ll get:
-
Evidence-based insights on training, performance, and recovery
-
Real analyses of supplements that work (and the ones that don’t)
-
Deep dives into hormones, nutrition, and human optimization
No fluff. No marketing hype. Just data-driven knowledge to build a stronger body — and a sharper mind.
Subscribe now and start mastering your biology.