In recent years, few drugs have generated as much buzz as Ozempic and Mounjaro. They’ve gone viral on social media, flooded clinics, and become part of everyday health conversations. But beyond the hype, what does the science actually say? Let’s break down what these drugs are, how they work, who should use them — and who definitely shouldn’t.
What Are Ozempic and Mounjaro?
Ozempic (semaglutide) and Mounjaro (tirzepatide) are injectable prescription medications originally developed to treat type 2 diabetes. Both belong to a class of drugs known as incretin mimetics, which act on hormones involved in regulating blood sugar and appetite.
- Ozempic mimics a natural hormone called GLP-1 (glucagon-like peptide-1).
- Mounjaro mimics two hormones — GLP-1 and GIP (glucose-dependent insulinotropic polypeptide) — giving it a potentially stronger effect on weight reduction and glucose control.
Although designed for diabetes, their remarkable weight-loss effects have made them a global phenomenon, driving massive off-label use among non-diabetic individuals.
How Do They Work?
GLP-1 and GIP are gut-derived hormones released after eating. They tell your brain that you’re full, slow down stomach emptying, and help the pancreas release insulin.
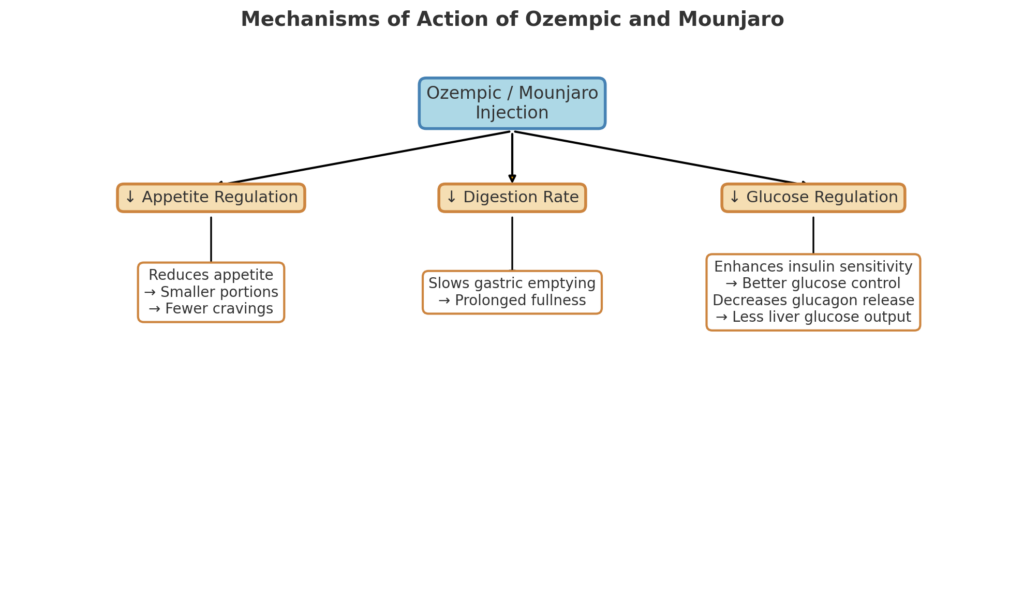
By mimicking these hormones, Ozempic and Mounjaro:
- Reduce appetite — leading to smaller meal portions and fewer cravings.
- Slow digestion — causing a prolonged feeling of fullness.
- Enhance insulin sensitivity — improving blood-sugar control.
- Decrease glucagon release — reducing liver glucose output.
The end result: less hunger, lower caloric intake, and gradual weight loss, often accompanied by improvements in blood sugar, cholesterol, and blood pressure.
What Has Science Proven About Them?
Numerous peer-reviewed clinical trials have confirmed their effectiveness.
- Semaglutide (Ozempic/Wegovy): The STEP 1 trial (Wilding et al., 2021) showed an average weight loss of ~15% of body weight over 68 weeks in non-diabetic adults, compared with 2.4% for placebo.
- Tirzepatide (Mounjaro): The SURMOUNT-1 study (Jastreboff et al., 2022) reported an even more impressive 20–22.5% reduction in body weight over 72 weeks — rivaling the results of bariatric surgery.
Beyond weight loss, both drugs improve insulin resistance, cardiovascular risk markers, and fatty-liver parameters (Sattar et al., 2023).
However, long-term data are still emerging. Most studies cover one to two years; little is known about what happens after five or ten years of continuous use.
Why Are They So Trending Today?
Three main reasons explain the hype:
- Social media virality: Celebrities, influencers, and even CEOs have openly discussed using these drugs for weight loss, fueling global curiosity.
- Unprecedented results: For decades, no pharmacological intervention came close to the effectiveness of these new incretin therapies.
- Aesthetic culture: Modern society prizes slimness, and people are willing to pay high prices for rapid results — often without considering long-term implications.
In short: they deliver visible transformation fast, and in a world obsessed with appearance, that’s a powerful selling point.
Who Should Use (and Who Shouldn’t)
✅ Recommended For
- Adults with type 2 diabetes inadequately controlled by diet and oral medication.
- Individuals with obesity (BMI ≥ 30) or overweight (BMI ≥ 27) with at least one weight-related condition (hypertension, dyslipidemia, prediabetes).
- Patients who have tried lifestyle interventions — diet and exercise — with insufficient results.
❌ Not Recommended For
- Individuals with a personal or family history of medullary thyroid carcinoma or MEN type 2 syndrome.
- Those with severe gastrointestinal disease (e.g., gastroparesis).
- Pregnant or breastfeeding women.
- People seeking purely aesthetic weight loss without medical supervision.
Misuse or abrupt discontinuation may lead to muscle loss, metabolic slowdown, and rapid weight regain — often worse than the starting point.
What Is “Ozempic Face”?
The term “Ozempic face” was coined by dermatologists and plastic surgeons to describe the sudden aging appearance some users report after rapid weight loss induced by GLP-1 medications.
When people lose fat quickly — especially facial fat — the volume beneath the skin decreases, leading to:
- Sagging or loose skin,
- More visible wrinkles and fine lines,
- A hollowed or tired appearance around the eyes and cheeks.
It’s not a side effect of the drug itself, but a consequence of drastic fat loss.
Facial fat acts as a natural filler that gives youthful contour to the face; when it disappears suddenly, skin elasticity may not keep up.
Experts emphasize that this effect can be mitigated by:
- Slower, controlled weight loss,
- Adequate protein intake,
- Strength training to maintain collagen and muscle support,
- Proper hydration and, in some cases, aesthetic interventions like fillers or skin tightening.
In essence, “Ozempic face” is more about how you lose weight than what you use to lose it.
Is This the Best Solution?
These drugs can be life-changing for individuals with obesity or metabolic disease, but they are not a magic bullet.
They work best when paired with:
- Nutrient-dense diets rich in protein and fiber,
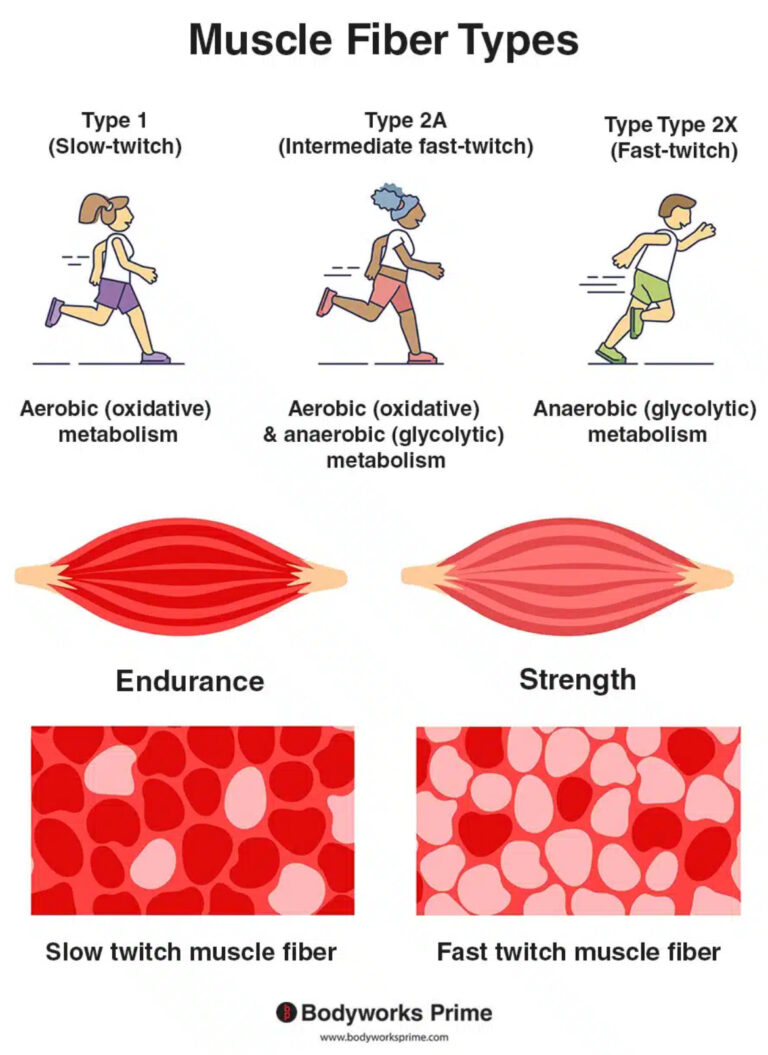
- Resistance training to preserve lean mass,
- Regular follow-ups with healthcare professionals.
Think of them as powerful tools, not replacements for discipline or lifestyle reform. They can jump-start progress, but long-term success still depends on habits.
Pros and Cons
| Pros | Cons |
|---|---|
| Clinically proven significant weight loss | Gastrointestinal side effects (nausea, vomiting, constipation) |
| Improves blood sugar control and insulin sensitivity | High cost, often not covered by insurance |
| Reduces cardiovascular risk factors | Potential muscle and lean-mass loss if not combined with resistance training |
| Lowers appetite and food cravings | Risk of rebound weight gain after discontinuation |
| May improve fatty-liver disease and inflammation | Limited long-term safety data |
| Once-weekly injection, easy compliance | Requires lifelong use for maintenance in most cases |
Final Thoughts
Ozempic and Mounjaro represent a revolution in metabolic medicine, bridging the gap between lifestyle changes and bariatric surgery. They offer hope for those who have struggled with obesity for years — but they also come with caveats.
Used responsibly and under medical supervision, they can transform health. Used recklessly, they can create dependency and disappointment.
The bottom line? If you choose to use them, do it smart — with science, not hype, guiding your decisions.
Forge Your Mind. Build Your Biology.
Join the Forge Biology newsletter — where science meets strength.
Every week, you’ll get:
-
Evidence-based insights on training, performance, and recovery
-
Real analyses of supplements that work (and the ones that don’t)
-
Deep dives into hormones, nutrition, and human optimization
No fluff. No marketing hype. Just data-driven knowledge to build a stronger body — and a sharper mind.
Subscribe now and start mastering your biology.